El Molloy, service user representative from Coventry & Warwickshire Maternity Voices Partnership, shares her report from the recent Westminster Policy Forum (WPF) keynote seminar on Maternity Services in England – patient safety, service delivery and policy priorities.
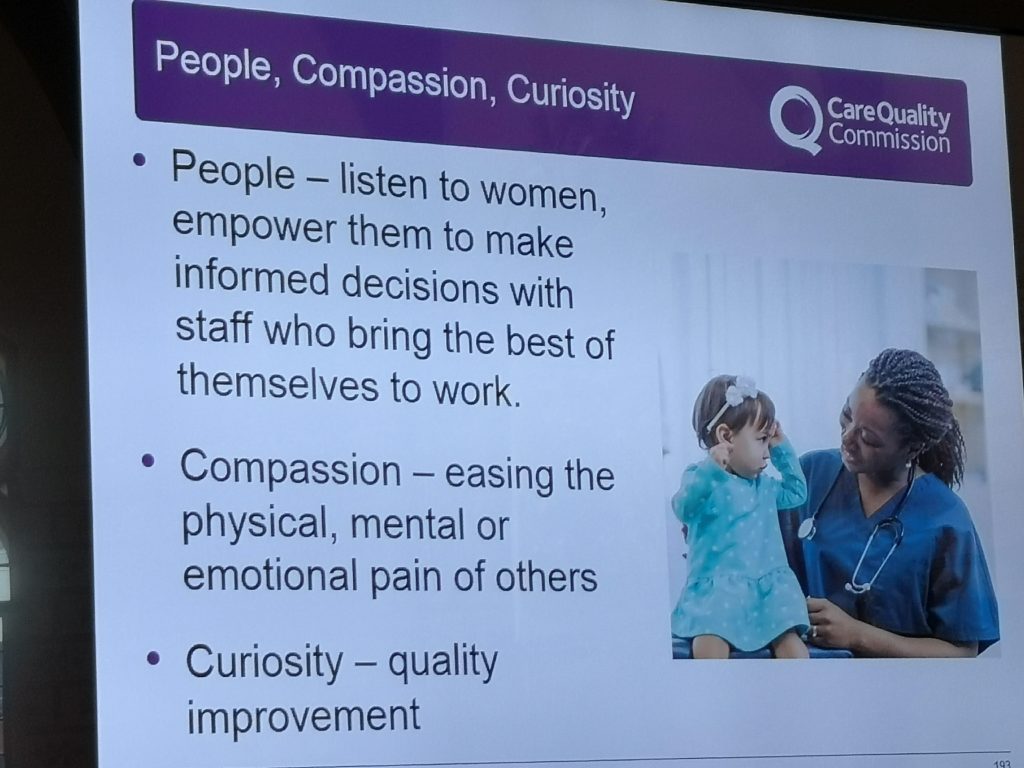
National Maternity Voices are delighted to hear recommendations from the Deputy chief inspector of hospitals at the Care Quality Commission, Dr Dr Nigel Acheson, on collaborating and coproducing with MVPs to improve maternity services. We urge all MVPs to make sure that you have access to local CQC data and work together to plan and see improvements as a result of the data.
Now over to El…
I was fortunate enough to be able to attend the WPF on Transforming Maternity Services on the 10th July in London, on behalf of National Maternity Voices. These events are run by a private company, they have multiple events on different policy areas that involve NHS/Social Care and Government; so will often be chaired by an MP with a special interest in the policy area, and/or other leaders from the voluntary sector.
 The format was a tightly scheduled morning session, other than the first speaker, the sessions were 3 speakers back to back, followed by 3 questions from the floor to the ‘panel’ (made up of the 3 speakers). The questions were asked together as a group, and then all three were answered.
The format was a tightly scheduled morning session, other than the first speaker, the sessions were 3 speakers back to back, followed by 3 questions from the floor to the ‘panel’ (made up of the 3 speakers). The questions were asked together as a group, and then all three were answered.
The session was chaired by Sharon Hodgson MP (Shadow Minister for Public Health, Vice-Chair All-Party Parliamentary Group on Baby Loss); and subsequently by Claire Mathews (Deputy Head of Maternity Services, NHS England).
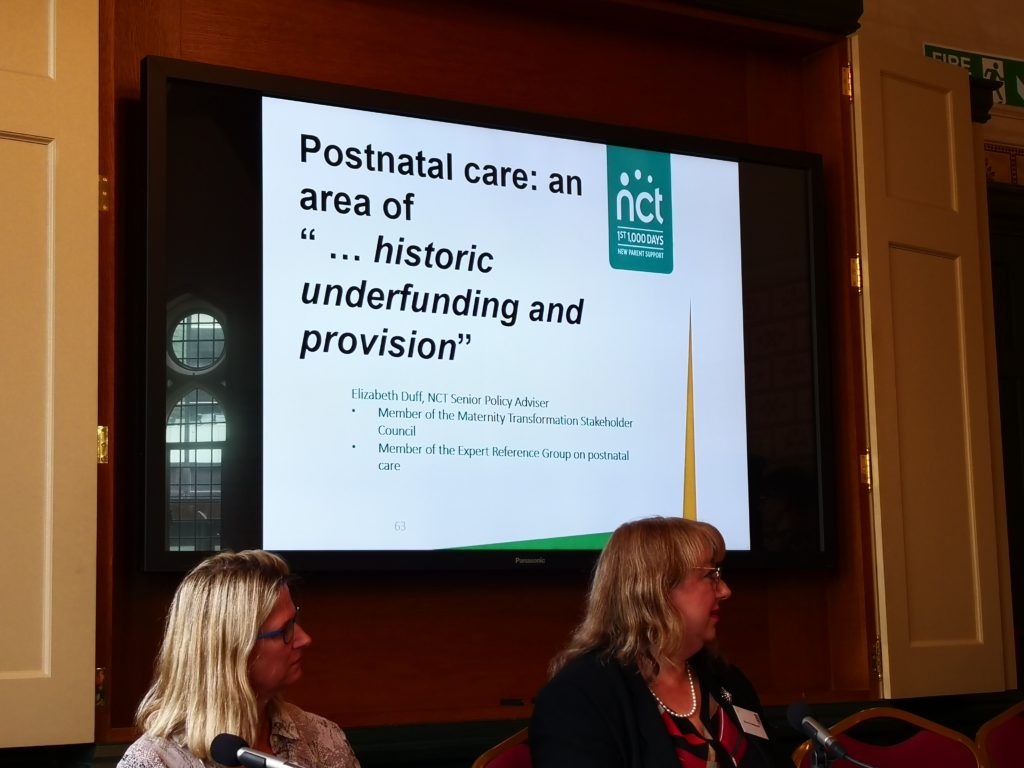
Speakers included Claire Mathews, Elizabeth Duff (Senior Policy Advisor, NCT); Linda Machakaire (Cons Midwife, Lewisham and Greenwich Trust); Prof. Heather O’Mahen (Ass Prof. and Perinatal Research Psychologist, Uni. Of Exeter); Clea Harmer (Chief Exec. Sands); Gill Walton (Chief Exec and Gen Sec. Royal College of Midwives) and Dr Nigel Acheson (Deputy Chief Insp. Of Hospitals, CQC).
My overall impression was that it was very much a session designed to facilitate networking and collaboration; and perhaps get people thinking more about cross-discipline working. The consensus from talking to people afterwards was they feel there have been positive steps taken, and that for some women, in some areas, accessibility and choice is improving. But the majority of the speakers really also focused on what needed to be done, and my hope is that when we start talking about good practice; it makes it easier to spot areas that are being left behind (or maybe I am too optimistic?!)
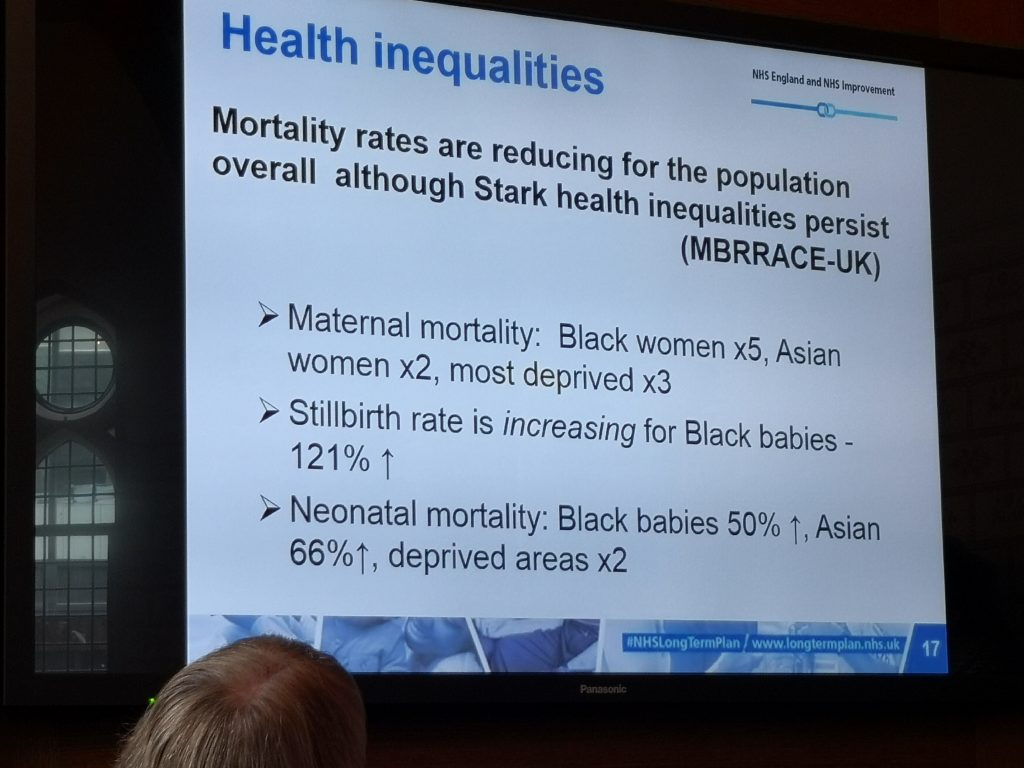
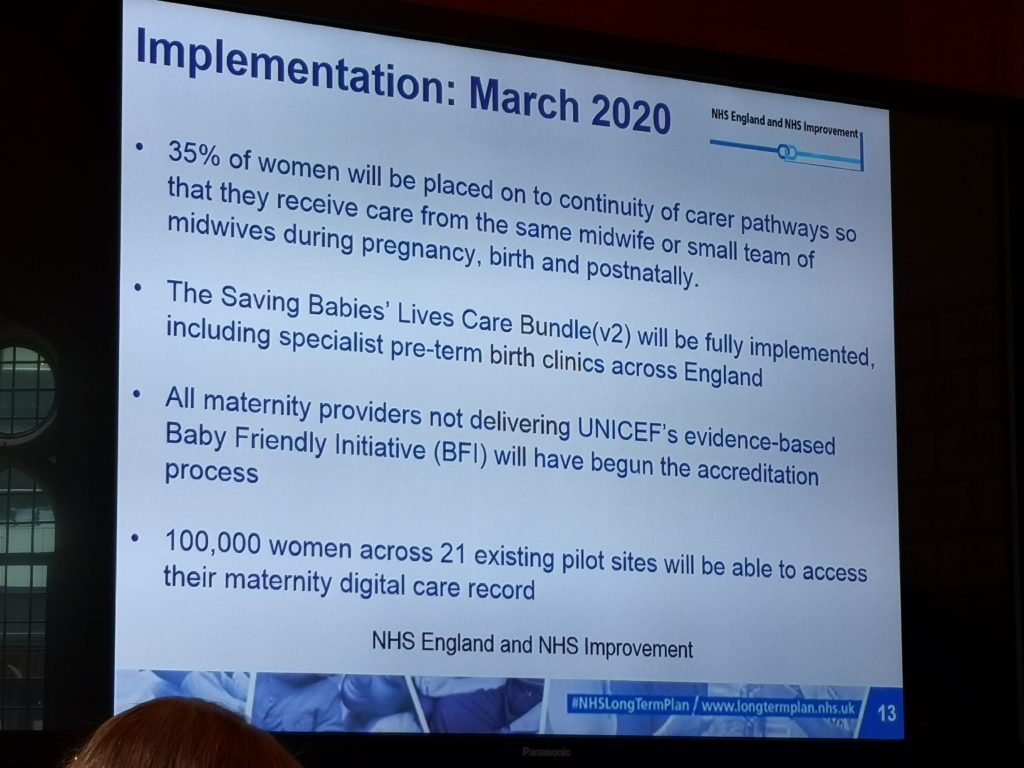
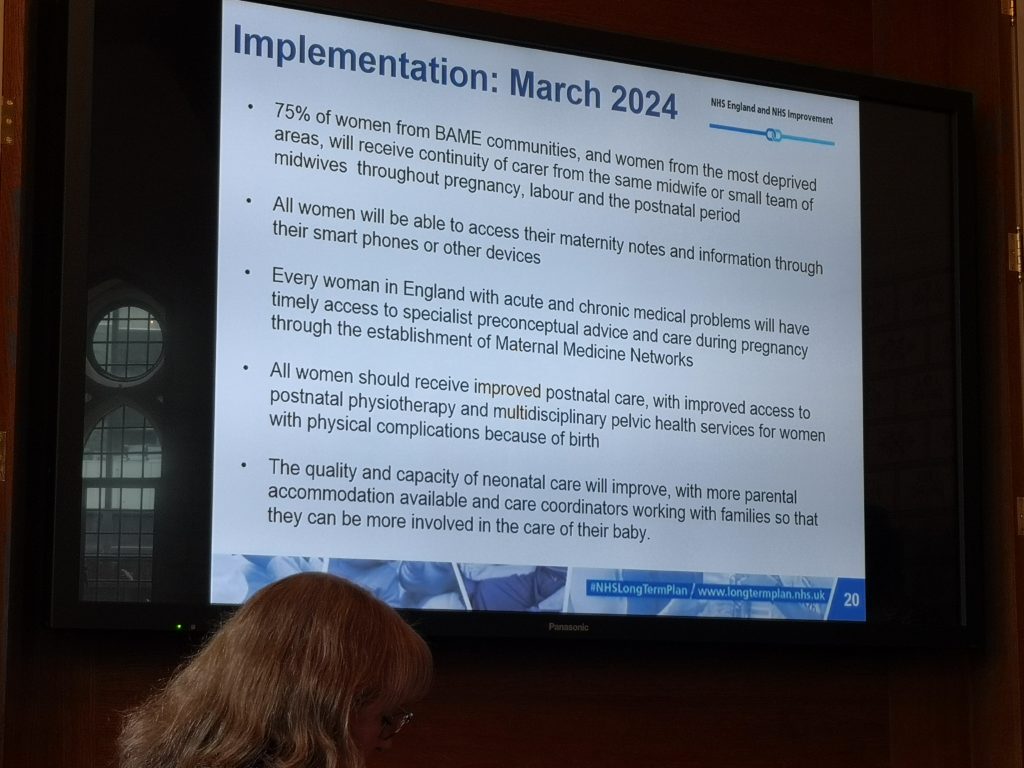
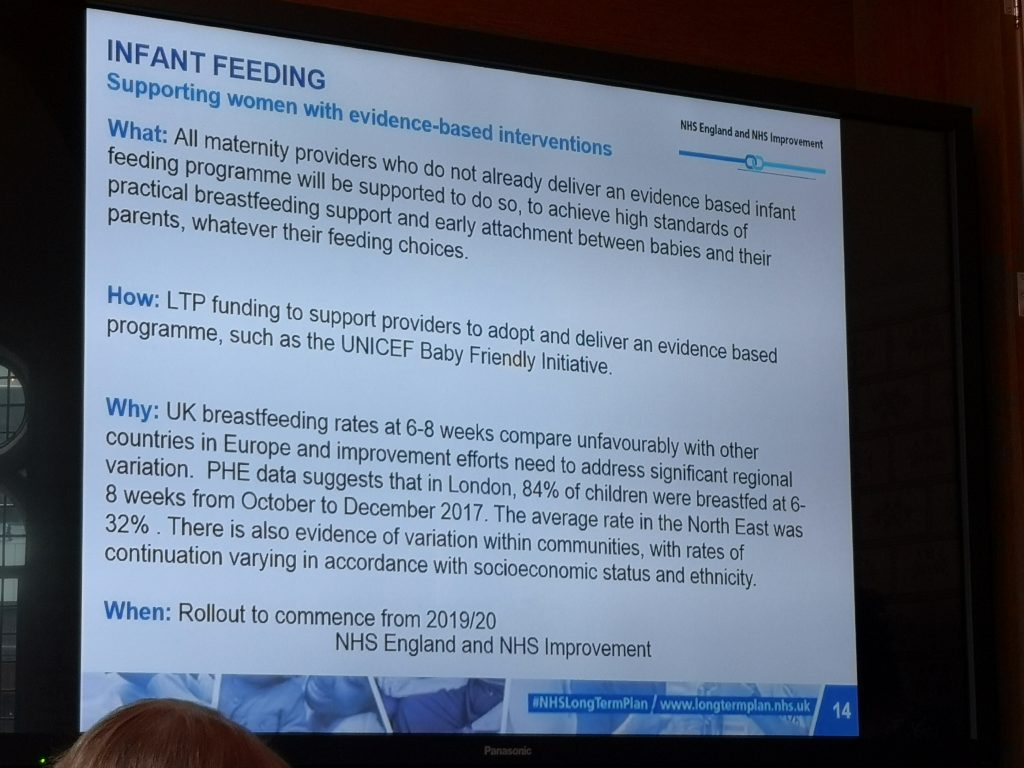
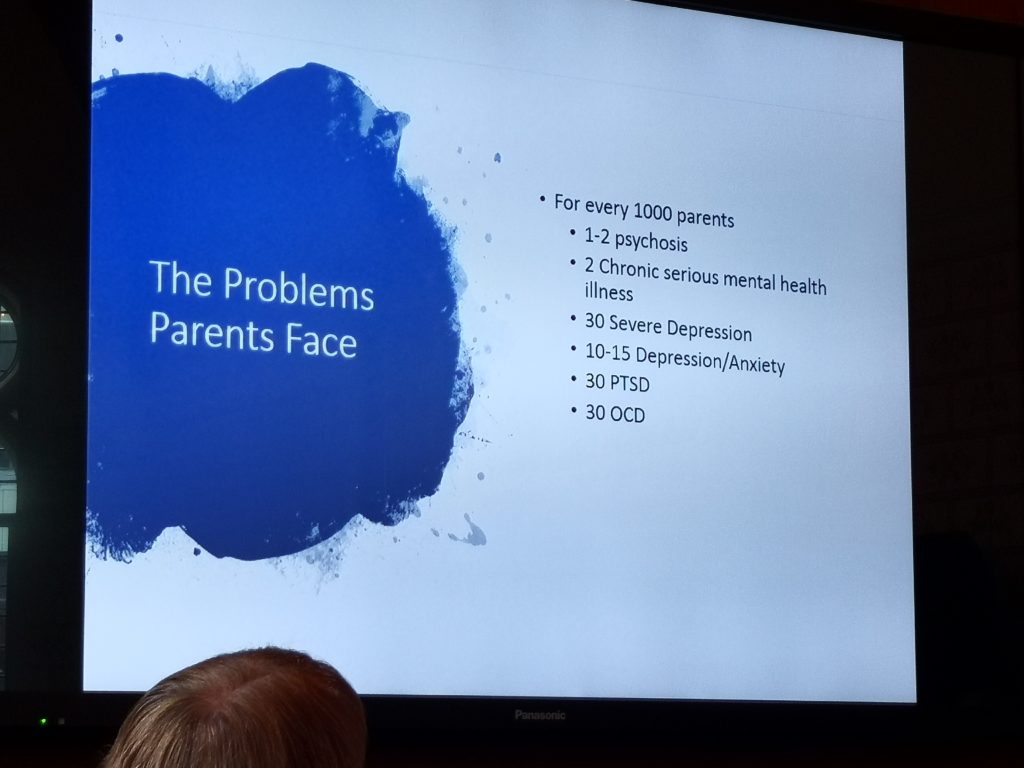
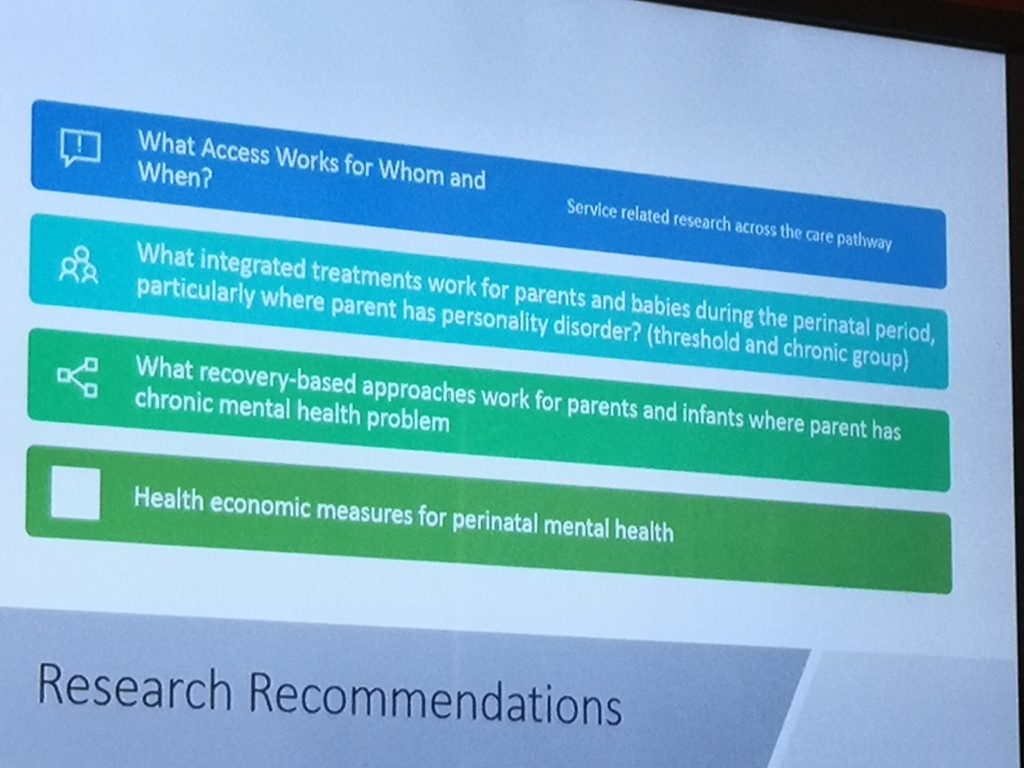
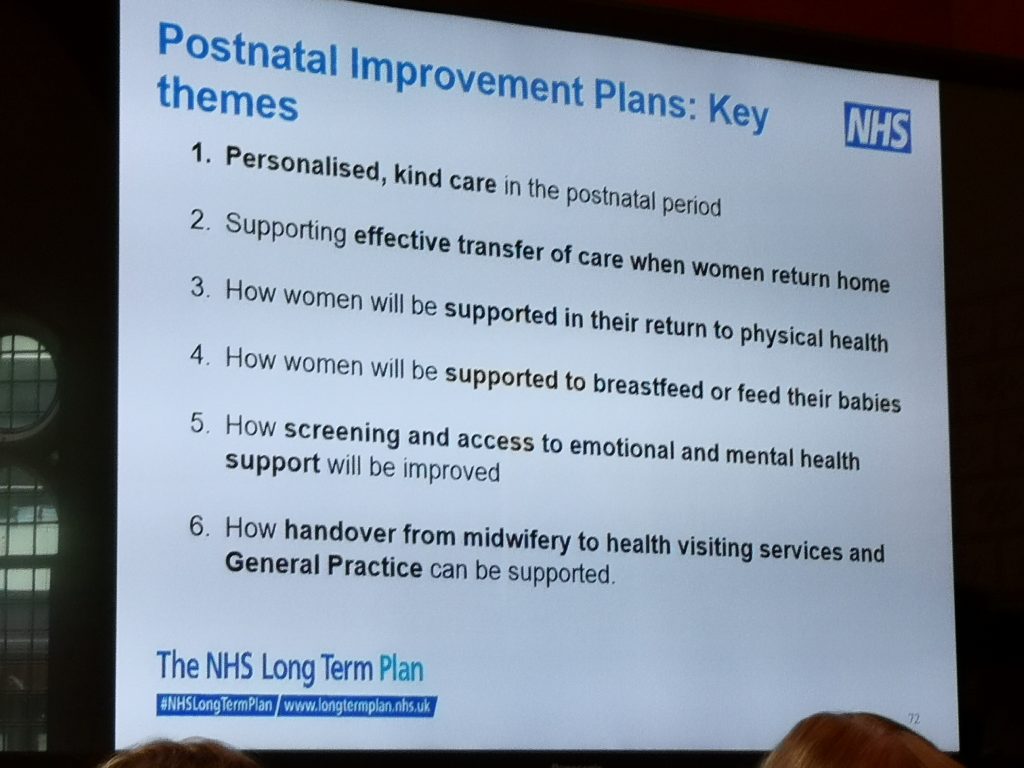
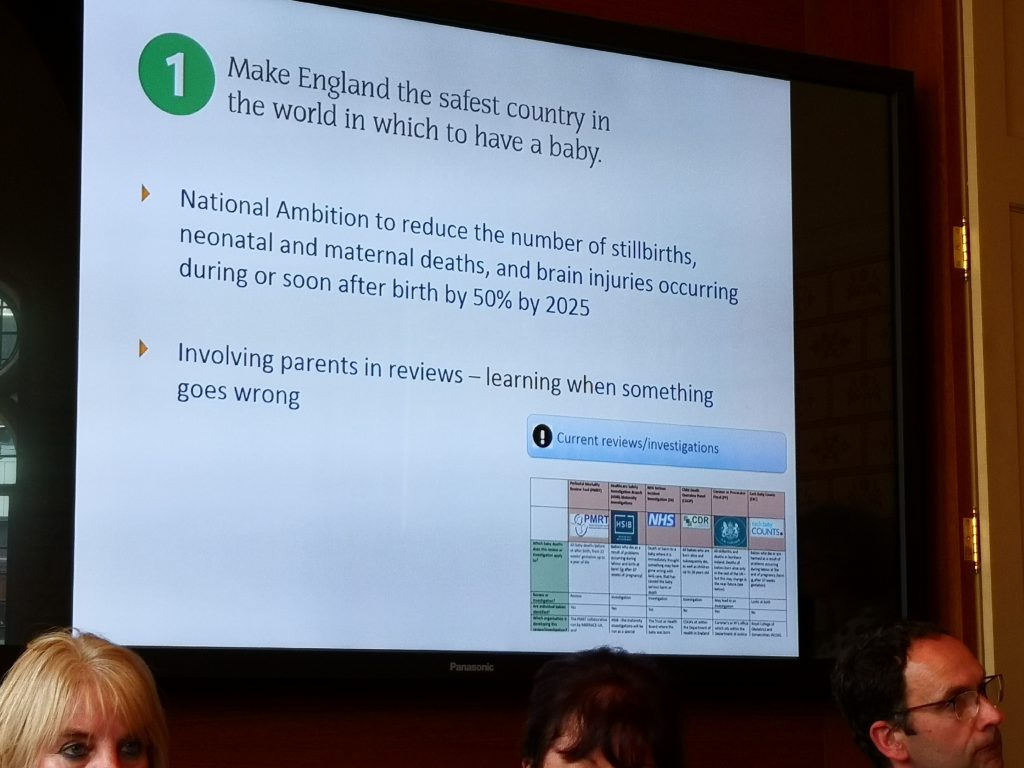
There was a focus from many of the speakers on the 50% reduction target for neonatal mortality and morbidity by 2025. Lots of plans in place around Perinatal Mental Health training modules for IAPT teams; integrating parent-infant services with adult services; bringing post-natal care into the maternal pathway rather than treating it as a separate (and poor) relation; increasing parental involvement in infant death reviews (where appropriate).
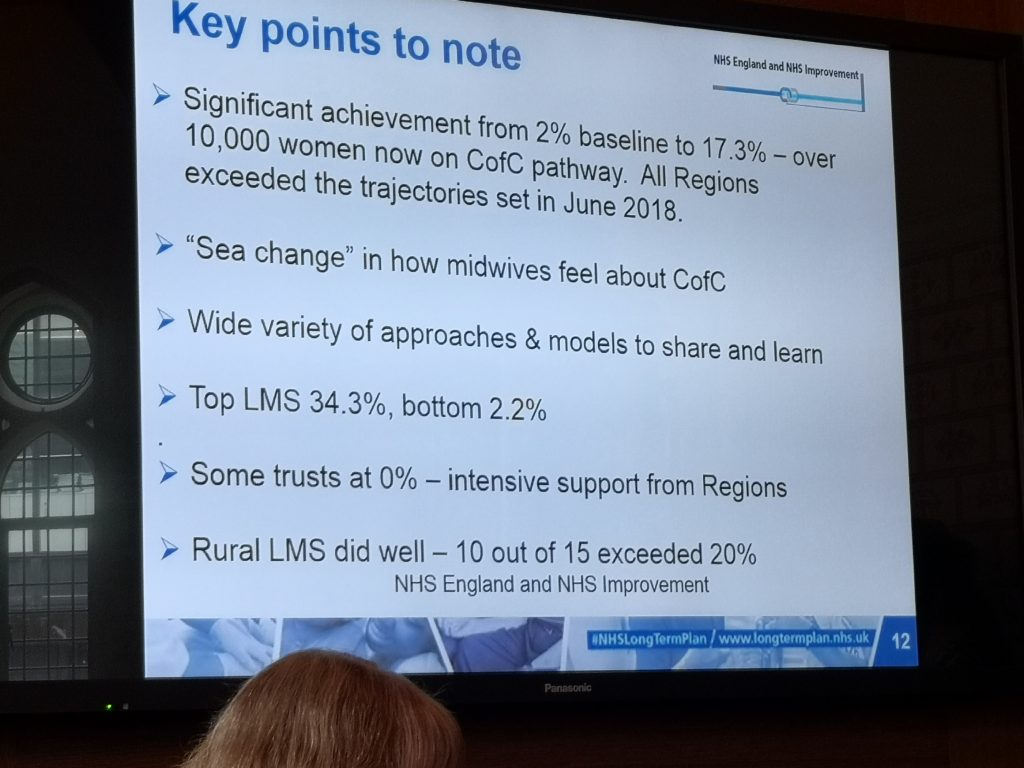
I had asked on the NMV and MVP groups about questions I could bring if the opportunity arose. Sadly there wasn’t scope to ask all of the questions I wanted to; but I did ask about strategies to improve Continuity of Care (CoC), and whether personalisation of care was being used in a way that actually meant women had true choice in their care. This seemed to be a tricky question to answer as the response seemed to be that overall it is hard to articulate cultural changes. There was also a perspective that the reticency on behalf of some staff to implement CoC was not always backed up by what the staff are actually saying, and that in some areas where one team has successfully implemented CoC, then there is an increased interest from other teams. Seems like this could be an area for some interesting qualitative research if there isn’t already some out there.
The presentation by Linda Machakaire was a really wonderful example of good, personalised care, that really focussed on listening to and supporting women who want to ‘birth outside of guidelines’ – there were key messages around caseloading and information sharing (using consultant midwife networks); discussing absolute risk (really liked her visual imagery about numbers of people in football stadiums); and that all of these discussions should be documented. Not only that but I thought a really interesting point was made about trusting colleagues – that if all of these discussions have taken place and a woman’s choice is still denied, what does that say about staff trust in their colleagues and peers?
The other really big take home message for me was in listening to the speaker from the CQC (Dr Nigel Acheson). Dr Acheson made a number of reference to Maternity Voices Partnerships – that as an organisation they expect to see maternity services engaging with the MVP in order to improve not just outcomes, but improve collaboration and co-production with service users and services. That if there are areas that require improvement within a setting, they would hope and expect that the MVP would be consulted in order to help work together to improve services.
There are a number of photos I took from slides below – I have a few more too! I could have written more about specific speakers, so if anyone wants to know more about any of the talks let me know. I am also waiting for the full sets of slides and the transcript of the session to be sent through.
Read more about the Westminster Policy Forum maternity event on twitter.